Coping With Achilles Tendinitis
Overview
 Achilles tendinitis is an overuse injury of the Achilles tendon, the band of tissue that connects calf muscles at the back of the lower leg to your heel bone. Achilles tendinitis most commonly occurs in runners who have suddenly increased the intensity or duration of their runs. It's also common in middle-aged people who play sports, such as tennis or basketball, only on the weekends. Most cases of Achilles tendinitis can be treated with relatively simple, at-home care under your doctor's supervision. Self-care strategies are usually necessary to prevent recurring episodes. More-serious cases of Achilles tendinitis can lead to tendon tears (ruptures) that may require surgical repair.
Achilles tendinitis is an overuse injury of the Achilles tendon, the band of tissue that connects calf muscles at the back of the lower leg to your heel bone. Achilles tendinitis most commonly occurs in runners who have suddenly increased the intensity or duration of their runs. It's also common in middle-aged people who play sports, such as tennis or basketball, only on the weekends. Most cases of Achilles tendinitis can be treated with relatively simple, at-home care under your doctor's supervision. Self-care strategies are usually necessary to prevent recurring episodes. More-serious cases of Achilles tendinitis can lead to tendon tears (ruptures) that may require surgical repair.
Causes
The calf is under a lot of strain when running: it is not only put on stretch during landing of the foot, but it also has to produce the tension needed to support body weight and absorb the shock of landing. This is what is called an ?eccentric load?. Excessive eccentric loading - either by way of a dramatic increase in mileage, or excessive hill running, or faulty running posture - could very well be the cause of a runner?s achilles tendinitis. The calf strain translates downward into the achilles tendon where it attaches to the heel, and inflammation ensues. Inflammation then causes scarring and fibrosis of tissues, which in turn inflicts pain upon stretching or use. Risk factors for Achilles tendinitis also include spending prolonged amounts of time standing or walking.
Symptoms
Common symptoms of Achilles tendinitis include weakness in the leg, slight pain above the heel in the lower leg after activity, feeling of stiffness in the leg that usually appears in the morning and lessens throughout the day, bad pain the day after exercising, pain as you climb stairs or go uphill, swelling in the area of the Achilles tendon, creaking or cracking noise when you press on the Achilles tendon.
Diagnosis
In diagnosing Achilles tendonitis or tendonosis, the surgeon will examine the patient?s foot and ankle and evaluate the range of motion and condition of the tendon. The extent of the condition can be further assessed with x-rays or other imaging modalities.
Nonsurgical Treatment
Physical therapy is the first and most useful defense for achilles tendonitis because of the two presentations outlined above. Treatments for the two types are quite different in approach. Midsubstance tendinitis responds well to stretching, whereas insertional tendnitis tends to be aggravated more by it. Depend on your trusted physical therapist to differentiate between the two and follow their guidelines on exercises and running modifications. Running gait patterns that show excessive ?sinking postures? tend to point to the source of achilles tendon problems. Altering your gait in the midstance phase of the cycle can reduce the load on the tendon dramatically and thereby reduce pain. Rely on your running physical therapist for proper guidance on altering your gait the right way. Stride Strong?s Portland Running Clinic gait analysis can identify and fix potential issues before pain sets in. Icing at the onset of acute achilles pain (i.e. when the injury is fresh and new) would help control the inflammation. Your next step should be to call our number for an appointment.
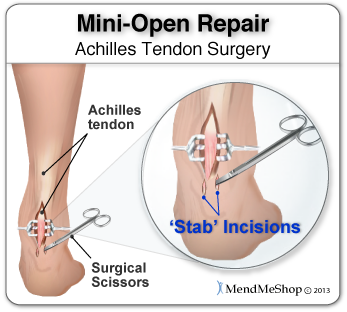
Surgical Treatment
Many people don't realize that Achilles tendon surgery can be very traumatic to your body. The type of trauma you experience after surgery can be compared to what you go through when you first injured your Achilles tendon. During the first 24 to 72 hours after the surgery your ankle will be tender, swollen and very painful. Your leg will be weak and unstable making it impossible for you to put weight on your leg without some kind of help. This is why your doctor or surgeon will have you outfitted for a cast, ankle brace and/or crutches before the procedure. When you are relying on a cast/brace and crutches your Achilles tendon is less likely to be as active as it once was. This is usually why atrophy (loss) of your lower leg muscles (specifically your calf muscle) happens. In general, more than 80%* of people who undergo surgery for an injured Achilles Tendon are able to return to their active lifestyle. In order to avoid re-injury, it is important to commit to a regular conservative therapy routine.
Prevention
A 2014 study looked at the effect of using foot orthotics on the Achilles tendon. The researchers found that running with foot orthotics resulted in a significant decrease in Achilles tendon load compared to running without orthotics. This study indicates that foot orthoses may act to reduce the incidence of chronic Achilles tendon pathologies in runners by reducing stress on the Achilles tendon1. Orthotics seem to reduce load on the Achilles tendon by reducing excessive pronation,
 Achilles tendinitis is an overuse injury of the Achilles tendon, the band of tissue that connects calf muscles at the back of the lower leg to your heel bone. Achilles tendinitis most commonly occurs in runners who have suddenly increased the intensity or duration of their runs. It's also common in middle-aged people who play sports, such as tennis or basketball, only on the weekends. Most cases of Achilles tendinitis can be treated with relatively simple, at-home care under your doctor's supervision. Self-care strategies are usually necessary to prevent recurring episodes. More-serious cases of Achilles tendinitis can lead to tendon tears (ruptures) that may require surgical repair.
Achilles tendinitis is an overuse injury of the Achilles tendon, the band of tissue that connects calf muscles at the back of the lower leg to your heel bone. Achilles tendinitis most commonly occurs in runners who have suddenly increased the intensity or duration of their runs. It's also common in middle-aged people who play sports, such as tennis or basketball, only on the weekends. Most cases of Achilles tendinitis can be treated with relatively simple, at-home care under your doctor's supervision. Self-care strategies are usually necessary to prevent recurring episodes. More-serious cases of Achilles tendinitis can lead to tendon tears (ruptures) that may require surgical repair.
Causes
The calf is under a lot of strain when running: it is not only put on stretch during landing of the foot, but it also has to produce the tension needed to support body weight and absorb the shock of landing. This is what is called an ?eccentric load?. Excessive eccentric loading - either by way of a dramatic increase in mileage, or excessive hill running, or faulty running posture - could very well be the cause of a runner?s achilles tendinitis. The calf strain translates downward into the achilles tendon where it attaches to the heel, and inflammation ensues. Inflammation then causes scarring and fibrosis of tissues, which in turn inflicts pain upon stretching or use. Risk factors for Achilles tendinitis also include spending prolonged amounts of time standing or walking.
Symptoms
Common symptoms of Achilles tendinitis include weakness in the leg, slight pain above the heel in the lower leg after activity, feeling of stiffness in the leg that usually appears in the morning and lessens throughout the day, bad pain the day after exercising, pain as you climb stairs or go uphill, swelling in the area of the Achilles tendon, creaking or cracking noise when you press on the Achilles tendon.
Diagnosis
In diagnosing Achilles tendonitis or tendonosis, the surgeon will examine the patient?s foot and ankle and evaluate the range of motion and condition of the tendon. The extent of the condition can be further assessed with x-rays or other imaging modalities.
Nonsurgical Treatment
Physical therapy is the first and most useful defense for achilles tendonitis because of the two presentations outlined above. Treatments for the two types are quite different in approach. Midsubstance tendinitis responds well to stretching, whereas insertional tendnitis tends to be aggravated more by it. Depend on your trusted physical therapist to differentiate between the two and follow their guidelines on exercises and running modifications. Running gait patterns that show excessive ?sinking postures? tend to point to the source of achilles tendon problems. Altering your gait in the midstance phase of the cycle can reduce the load on the tendon dramatically and thereby reduce pain. Rely on your running physical therapist for proper guidance on altering your gait the right way. Stride Strong?s Portland Running Clinic gait analysis can identify and fix potential issues before pain sets in. Icing at the onset of acute achilles pain (i.e. when the injury is fresh and new) would help control the inflammation. Your next step should be to call our number for an appointment.
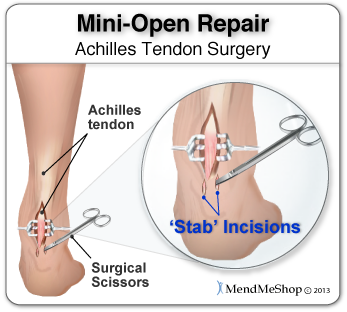
Surgical Treatment
Many people don't realize that Achilles tendon surgery can be very traumatic to your body. The type of trauma you experience after surgery can be compared to what you go through when you first injured your Achilles tendon. During the first 24 to 72 hours after the surgery your ankle will be tender, swollen and very painful. Your leg will be weak and unstable making it impossible for you to put weight on your leg without some kind of help. This is why your doctor or surgeon will have you outfitted for a cast, ankle brace and/or crutches before the procedure. When you are relying on a cast/brace and crutches your Achilles tendon is less likely to be as active as it once was. This is usually why atrophy (loss) of your lower leg muscles (specifically your calf muscle) happens. In general, more than 80%* of people who undergo surgery for an injured Achilles Tendon are able to return to their active lifestyle. In order to avoid re-injury, it is important to commit to a regular conservative therapy routine.
Prevention
A 2014 study looked at the effect of using foot orthotics on the Achilles tendon. The researchers found that running with foot orthotics resulted in a significant decrease in Achilles tendon load compared to running without orthotics. This study indicates that foot orthoses may act to reduce the incidence of chronic Achilles tendon pathologies in runners by reducing stress on the Achilles tendon1. Orthotics seem to reduce load on the Achilles tendon by reducing excessive pronation,
Complications Caused By Diabetic Feet
Persistent unilateral (one -sided) swelling of feet can be a sign of serious damage to the bones and joints of his feet and needs to be shown to a doctor immediately. If the foot wear is worn out at particular place, it is indicative of extra pressure being applied at that area of the foot and needs to be shown to the doctor at the earliest. While traveling, one must not remove his/her footwear and rest the feet on the floor of the vehicle. No amount of drugs/medicines can keep a patient's feet intact unless the patient is wearing properly designed footwear. All foot wear must always be worn with socks. It is necessary to avoid direct contact between the footwear and skin. Socks also help in reducing the damage to the skin of the fore foot. The heel of the foot should be completely supported by FULL HEEL COUNTER. Diabetic neuroischemic foot.

We understand that prevention needs to be a combination of systemic disease control and self foot-care, which includes proper foot hygiene, foot inspection and proper foot gear. As health care professionals, we are at a loss for effective methods to influence behaviors in our patients, especially because behaviors are difficult to address in the short period of time we have with them. Apparently intelligence has little to do with an inability to care for one's self, as many high functioning adults may have rather questionable personal habits. The study looked at 302 type II diabetics from the VA healthcare system in Taiwan divided into two groups; 155 received group lectures in addition to routine healthcare, and 147 received only routine care. A retrospective review of medical records and a structured interview were conducted to determine the foot care quality among the two groups. Epidemiology and prevention.
There is the specific broken ankle recovery occasion any particular one should know. This really is to help no cost your ex in the popular broken ankle recovery oversight that will other folks happen to be doing. Eventhough it can be simple to comprehend that you could really hope his or her foot to mend quick, she must likewise agree to the reality that broken ankle recovery moment probably won't match their preference.
Diabetic foot ulcers as one of the most common complications of diabetes mellitus are defined as nonhealing or long-lasting chronic skin ulcers in diabetic patients. Low level laser therapy (LLLT) on wound areas as well as on acupuncture points, as a noninvasive, pain-free method with minor side effects, has been considered as a possible treatment option for the diabetic foot syndrome. The majority of clinical studies show a potential benefit of LLLT in wound healing of diabetic ulcers.
Under normal circumstances, a blister created in this manner wouldn't present a health risk, but diabetics have poor circulation, putting them in danger of infection complications. The American Diabetes Association lists the infection as the fungal contagion most often found in those with diabetes. Candida albicans presents an itchy, red rash surrounded by blisters and scales that occur in warm, moist folds of skin - such as the area under breasts, between the fingers and toes, under the foreskin, in the armpits and groin. Prescription medication treats the fungal infection in diabetics, effectively clearing up the blisters.
Dyshidrotic eczema, which is also called vesicular eczema of hands or feet, is a form of eczema that is characterized by cracked skin and itchy blisters. The affected individual Foot Conditions must refrain from scratching over the affected skin. Psoriasis is a skin condition that is characterized by the development of inflamed patches of skin and silvery scales.


We understand that prevention needs to be a combination of systemic disease control and self foot-care, which includes proper foot hygiene, foot inspection and proper foot gear. As health care professionals, we are at a loss for effective methods to influence behaviors in our patients, especially because behaviors are difficult to address in the short period of time we have with them. Apparently intelligence has little to do with an inability to care for one's self, as many high functioning adults may have rather questionable personal habits. The study looked at 302 type II diabetics from the VA healthcare system in Taiwan divided into two groups; 155 received group lectures in addition to routine healthcare, and 147 received only routine care. A retrospective review of medical records and a structured interview were conducted to determine the foot care quality among the two groups. Epidemiology and prevention.
There is the specific broken ankle recovery occasion any particular one should know. This really is to help no cost your ex in the popular broken ankle recovery oversight that will other folks happen to be doing. Eventhough it can be simple to comprehend that you could really hope his or her foot to mend quick, she must likewise agree to the reality that broken ankle recovery moment probably won't match their preference.
Diabetic foot ulcers as one of the most common complications of diabetes mellitus are defined as nonhealing or long-lasting chronic skin ulcers in diabetic patients. Low level laser therapy (LLLT) on wound areas as well as on acupuncture points, as a noninvasive, pain-free method with minor side effects, has been considered as a possible treatment option for the diabetic foot syndrome. The majority of clinical studies show a potential benefit of LLLT in wound healing of diabetic ulcers.
Under normal circumstances, a blister created in this manner wouldn't present a health risk, but diabetics have poor circulation, putting them in danger of infection complications. The American Diabetes Association lists the infection as the fungal contagion most often found in those with diabetes. Candida albicans presents an itchy, red rash surrounded by blisters and scales that occur in warm, moist folds of skin - such as the area under breasts, between the fingers and toes, under the foreskin, in the armpits and groin. Prescription medication treats the fungal infection in diabetics, effectively clearing up the blisters.
Dyshidrotic eczema, which is also called vesicular eczema of hands or feet, is a form of eczema that is characterized by cracked skin and itchy blisters. The affected individual Foot Conditions must refrain from scratching over the affected skin. Psoriasis is a skin condition that is characterized by the development of inflamed patches of skin and silvery scales.
What Brings About Plantar Fasciitis And The Ways To Cure It

Overview
The plantar fascia (a connective tissue structure) stretches from the toes and ball of the foot, through the arch, and connects to the heel bone in three places: outside, center and inside. Normally it helps the foot spring as it rolls forward. It also provides support for the arch of the foot. The plantar fascia helps keep the foot on track, cutting down on oscillation. When the foot over-pronates (rolls to the inside) the plantar fascia tries to stabilize it and prevent excessive roll. In time, the inside and sometimes center connections are overstressed and pull away from their attachments. The first sign is usually heel pain as you rise in the morning. When you walk around, the pain may subside, only to return the next morning. Inflammation and increased soreness are the results of long-term neglect and continued abuse. A heel bone spur may develop after a long period of injury when there is no support for the heel. The plantar fascia attaches to the heel bone with small fibers. When these become irritated they become inflamed with blood containing white blood cells. Within the white blood cells are osteoblasts which calcify to form bone spurs and calcium deposits. The body is trying to reduce stress on that area by building a bone in the direction of stress. Unfortunately, these foreign substances cause pain and further irritation in the surrounding soft tissue.
Causes
Plantar fasciitis generally occurs over time, rather than being the result of a single event. Micro trauma from repetitive stress to the tissue often combines with a biomechanical deficiency of the foot to produce the condition. In addition, arthritic and metabolic factors may contribute to the development of this injury, (though they are unlikely to affect young athletes). A variety of training errors commonly lead to plantar fasciitis, particularly a rapid increase in either volume or intensity of athletic activity. Volume refers to the distance or time an athlete performs, while intensity refers to the pace of activity and/or the recovery time allowed following performance.
Symptoms
The most common symptom is pain and stiffness in the bottom of the heel. The heel pain may be dull or sharp. The bottom of the foot may also ache or burn. The pain is often worse in the morning when you take your first steps, after standing or sitting for awhile, when climbing stairs, after intense activity. The pain may develop slowly over time, or come on suddenly after intense activity.
Diagnosis
X-rays are a commonly used diagnostic imaging technique to rule out the possibility of a bone spur as a cause of your heel pain. A bone spur, if it is present in this location, is probably not the cause of your pain, but it is evidence that your plantar fascia has been exerting excessive force on your heel bone. X-ray images can also help determine if you have arthritis or whether other, more rare problems, stress fractures, bone tumors-are contributing to your heel pain.
Non Surgical Treatment
Treatment initially involves offloading the plantar fascia by aoiding aggravating factors, such as running. Taping, this can work very well to alleviate pain, and can be almost immediate. It isn't a long-term solution, but can relieve symptoms in the beginning. Using a night splint to stretch the calf, so that less load is placed on the plantar fascia (if tightness in the calf is a factor). Using a gel heel cup, this can act to increase shock absorption, and by raising the heel there is also less stretch on the calf. So, temporarily, this may relieve pain in someone who has a tight calf. Massage, but this depends if the plantarfascia is actually tight or just painful. If it is tight, then massage can temporarily relieve the pain, but if it is irritated then taping and corrective footwear is preferable.

Surgical Treatment
Most practitioners agree that treatment for plantar fasciitis is a slow process. Most cases resolve within a year. If these more conservative measures don't provide relief after this time, your doctor may suggest other treatment. In such cases, or if your heel pain is truly debilitating and interfering with normal activity, your doctor may discuss surgical options with you. The most common surgery for plantar fasciitis is called a plantar fascia release and involves releasing a portion of the plantar fascia from the heel bone. A plantar fascia release can be performed through a regular incision or as endoscopic surgery, where a tiny incision allows a miniature scope to be inserted and surgery to be performed. About one in 20 patients with plantar fasciitis will need surgery. As with any surgery, there is still some chance that you will continue to have pain afterwards.
Stretching Exercises
The following exercises are commonly prescribed to patients with this condition. You should discuss the suitability of these exercises with your physiotherapist prior to beginning them. Generally, they should be performed 2 - 3 times daily and only provided they do not cause or increase symptoms. Your physiotherapist can advise when it is appropriate to begin the initial exercises and eventually progress to the intermediate and advanced exercises. As a general rule, addition of exercises or progression to more advanced exercises should take place provided there is no increase in symptoms. Calf Stretch with Towel. Begin this stretch in long sitting with your leg to be stretched in front of you. Your knee and back should be straight and a towel or rigid band placed around your foot as demonstrated. Using your foot, ankle and the towel, bring your toes towards your head until you feel a stretch in the back of your calf, Achilles tendon, plantar fascia or leg. Hold for 5 seconds and repeat 10 times at a mild to moderate stretch provided the exercise is pain free. Resistance Band Calf Strengthening. Begin this exercise with a resistance band around your foot as demonstrated and your foot and ankle held up towards your head. Slowly move your foot and ankle down against the resistance band as far as possible and comfortable without pain, tightening your calf muscle. Very slowly return back to the starting position. Repeat 10 - 20 times provided the exercise is pain free.
What Is Heel Pain
Overview
Plantar fasciitis is the most common cause of heel pain. The plantar fascia is the flat band of tissue (ligament) that connects your heel bone to your toes. It supports the arch of your foot. If you strain your plantar fascia, it gets weak, swollen, and irritated (inflamed). Then your heel or the bottom of your foot hurts when you stand or walk. Plantar fasciitis is common in middle-aged people. It also occurs in younger people who are on their feet a lot, like athletes or soldiers. It can happen in one foot or both feet.
Causes
Plantar fasciitis is caused by straining the ligament that supports your arch. Repeated strain can cause tiny tears in the ligament. These can lead to pain and swelling. This is more likely to happen if your feet roll inward too much when you walk ( excessive pronation ). You have high arches or flat feet. You walk, stand, or run for long periods of time, especially on hard surfaces. You are overweight. You wear shoes that don't fit well or are worn out. You have tight Achilles tendons or calf muscles.
Symptoms
A sharp pain in the center of your heel will most likely be one of the biggest symptoms of plantar fasciitis. A classic sign of plantar fasciitis is when the pain is worst during the first steps you take in the morning.
Diagnosis
Plantar fasciosis is confirmed if firm thumb pressure applied to the calcaneus when the foot is dorsiflexed elicits pain. Fascial pain along the plantar medial border of the fascia may also be present. If findings are equivocal, demonstration of a heel spur on x-ray may support the diagnosis; however, absence does not rule out the diagnosis, and visible spurs are not generally the cause of symptoms. Also, infrequently, calcaneal spurs appear ill defined on x-ray, exhibiting fluffy new bone formation, suggesting spondyloarthropathy (eg, ankylosing spondylitis, reactive arthritis. If an acute fascial tear is suspected, MRI is done.
Non Surgical Treatment
A doctor may prescribe anti-inflammatory medication such as ibuprofen to help reduce pain and inflammation. Electrotherapy such as ultrasound or laser may also help with symptoms. An X-ray may be taken to see if there is any bone growth or calcification, known as a heel spur but this is not necessarily a cause of pain. Deep tissue sports massage techniques can reduce the tension in and stretch the plantar fascia and the calf muscles. Extracorporeal shock wave therapy has been known to be successful and a corticosteroid injection is also an option.

Surgical Treatment
Plantar fasciotomy is often considered after conservative treatment has failed to resolve the issue after six months and is viewed as a last resort. Minimally invasive and endoscopic approaches to plantar fasciotomy exist but require a specialist who is familiar with certain equipment. Heel spur removal during plantar fasciotomy has not been found to improve the surgical outcome. Plantar heel pain may occur for multiple reasons and release of the lateral plantar nerve branch may be performed alongside the plantar fasciotomy in select cases. Possible complications of plantar fasciotomy include nerve injury, instability of the medial longitudinal arch of the foot, fracture of the calcaneus, prolonged recovery time, infection, rupture of the plantar fascia, and failure to improve the pain. Coblation (TOPAZ) surgery has recently been proposed as alternative surgical approaches for the treatment of recalcitrant plantar fasciitis.
What Is Plantar Fasciitis
Overview
Plantar fasciitis is characterized by stiffness and inflammation of the main fascia (fibrous connective [ligament-like] tissue) on the bottom of the foot. It is occasionally associated with a bone spur on the heel. Occasionally there may be a partial or complete tear of the fascia of the bottom of the foot. Bone spurs themselves usually do not cause symptoms.
Causes
The cause of plantar fasciitis is poorly understood and is thought to likely have several contributing factors. The plantar fascia is a thick fibrous band of connective tissue that originates from the medial tubercle and anterior aspect of the heel bone. From there, the fascia extends along the sole of the foot before inserting at the base of the toes, and supports the arch of the foot. Originally, plantar fasciitis was believed to be an inflammatory condition of the plantar fascia. However, within the last decade, studies have observed microscopic anatomical changes indicating that plantar fasciitis is actually due to a non-inflammatory structural breakdown of the plantar fascia rather than an inflammatory process. Due to this shift in thought about the underlying mechanisms in plantar fasciitis, many in the academic community have stated the condition should be renamed plantar fasciosis. The structural breakdown of the plantar fascia is believed to be the result of repetitive microtrauma (small tears). Microscopic examination of the plantar fascia often shows myxomatous degeneration, connective tissue calcium deposits, and disorganized collagen fibers. Disruptions in the plantar fascia’s normal mechanical movement during standing and walking (known as the Windlass mechanism) are thought to contribute to the development of plantar fasciitis by placing excess strain on the calcaneal tuberosity.
Symptoms
You'll typically first notice early plantar fasciitis pain under your heel or in your foot arch in the morning or after resting. Your heel pain will be worse with the first steps and improves with activity as it warms up. As plantar fasciitis deteriorates, the pain will be present more often. You can determine what stage your are in using the following guidelines. No Heel Pain, Normal! Heel pain after exercise. Heel pain before and after exercise. Heel pain before, during and after exercise. Heel pain all the time. Including at rest! This symptom progression is consistent with the four stages of a typical overuse injury. Ultimately, further trauma and delayed healing will result in the formation of calcium (bone) within the plantar fascia. When this occurs adjacent to the heel bone it is known as heel spurs, which have a longer rehabilitation period.
Diagnosis
Plantar fasciitis is one of many conditions causing "heel pain". Some other possible causes include nerve compression either in the foot or in the back, stress fracture of the calcaneus, and loss of the fatty tissue pad under the heel. Plantar fasciitis can be distinguished from these and other conditions based on a history and examination done by a physician. It should be noted that heel spurs are often inappropriately thought to be the sole cause of heel pain. In fact, heel spurs are common and are nothing more than the bone's response to traction or pulling-type forces from the plantar fascia and other muscles in the foot where they attach to the heel bone. They are commonly present in patients without pain, and frequently absent from those who have pain. It is the rare patient who has a truly enlarged and problematic spur requiring surgery.
Non Surgical Treatment
The initial treatment of plantar fasciitis focuses on reducing pain and inflammation. Resting the affected foot is the most important aspect of this treatment. Other initial treatment may include, aplying ice to the sole of the foot, Anti-inflammatory medications. Gentle stretching of the plantar fascia and Achilles tendon. Physiotherapy. Taping the foot and ankle to provide adequate support and alignment, Wearing supportive footwear with shock-absorbing soles or inserts. Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Brufen) and diclofenac (Voltaren) are often used to treat plantar fasciitis. It is unclear whether NSAIDs assist in the healing process but they are useful for controlling pain during treatment. If the condition does not respond to initial treatment, a corticosteroid therapy may be recommended. This involves the injection of corticosteroid medication such as hydrocortisone (Solu-Cortef) directly into the affected area in order to treat the inflammation and thus relieve the pain. Night splints to prevent the plantar fascia tightening during sleep may also be recommended at this stage.

Surgical Treatment
Like every surgical procedure, plantar fasciitis surgery carries some risks. Because of these risks your doctor will probably advise you to continue with the conventional treatments at least 6 months before giving you approval for surgery. Some health experts recommend home treatment as long as 12 months. If you can’t work because of your heel pain, can’t perform your everyday activities or your athletic career is in danger, you may consider a plantar fasciitis surgery earlier. But keep in mind that there is no guarantee that the pain will go away completely after surgery. Surgery is effective in many cases, however, 20 to 25 percent of patients continue to experience heel pain after having a plantar fasciitis surgery.
Prevention
To reduce your risk of getting plantar fasciitis take these steps. Wear appropriate and well-fitted footwear during sports and exercise. Do stretching exercises for the Achilles tendon and plantar fascia. Increase the intensity and duration of exercise gradually. Maintain an appropriate weight.
Achilles Tendonitis
Overview
 Achilles tendonitis is commonly seen in athletes who sustain an increase in training load, and is most often due to overuse. Tendons respond poorly to overuse, therefore healing is slow. This can leave a tendon pathologically defective, which decreases tendon strength and leaves it less able to tolerate load, thus vulnerable to further injury or tendinosis. Extrinsic factors contributing to this condition include training errors and inappropriate footwear. Intrinsic factors include inflexibility, weakness and malalignment. In other situations, there will be clinical inflammation, but objective pathologic evidence for cellular inflammation is lacking, and in these conditions the term tendinosis is more appropriate. Tendinosis is a degeneration of the tendon?s collagen in response to chronic overuse; when overuse is continued without giving the tendon time to heal and rest, such as with repetitive strain injury, tendinosis results. Even tiny movements, such as clicking a mouse, can cause tendinosis, when done repeatedly.
Achilles tendonitis is commonly seen in athletes who sustain an increase in training load, and is most often due to overuse. Tendons respond poorly to overuse, therefore healing is slow. This can leave a tendon pathologically defective, which decreases tendon strength and leaves it less able to tolerate load, thus vulnerable to further injury or tendinosis. Extrinsic factors contributing to this condition include training errors and inappropriate footwear. Intrinsic factors include inflexibility, weakness and malalignment. In other situations, there will be clinical inflammation, but objective pathologic evidence for cellular inflammation is lacking, and in these conditions the term tendinosis is more appropriate. Tendinosis is a degeneration of the tendon?s collagen in response to chronic overuse; when overuse is continued without giving the tendon time to heal and rest, such as with repetitive strain injury, tendinosis results. Even tiny movements, such as clicking a mouse, can cause tendinosis, when done repeatedly.
Causes
Like any muscle or tendon in the body, the older we get, the more likely we are to sustain an injury. So middle-aged men and women are most at risk, with a slightly higher risk factor attributed to males. Those who participate in more intense athletic activities like high impact sports (tennis, running, basketball) are most susceptible to the injury. Certain underlying medical conditions can also be a contributing factor. Diabetics are more at risk of suffering from Achilles Tendinitis, as are those who are not in great physical shape. Some antibiotics, particularly fluoroquinolones can make one more likely to suffer a strained Achilles Tendon.
Symptoms
Symptoms vary because you can injure various areas of the muscle-tendon complex. The pain may be an acute or chronic sharp, stabbing, piercing, shooting, burning or aching. It is often most noticeable immediately after getting out of bed in the morning, or after periods of inactivity, like sitting down for lunch. After a couple minutes of walking around, it will often then settle down somewhat, before becoming symptomatic again after excessive time standing or walking. But regardless of how the pain is perceived, Achilles tendon pain should not be left untreated due to the danger that the tendon can become weak, frayed, thickened, and eventually it may rupture.
Diagnosis
On examination, an inflamed or partially torn Achilles tendon is tender when squeezed between the fingers. Complete tears are differentiated by sudden, severe pain and inability to walk on the extremity. A palpable defect along the course of the tendon. A positive Thompson test (while the patient lies prone on the examination table, the examiner squeezes the calf muscle; this maneuver by the examiner does not cause the normally expected plantar flexion of the foot).
Nonsurgical Treatment
Treatment depends on severity of pain. The most effective long-term treatment for Achilles tendinitis/tendinopathy is physical therapy, particularly therapy that focuses on eccentric muscle/tendon strengthening. Calf and Achilles stretching are also an important part of the treatment. In severe cases, treatment may begin with a period of rest and immobilization in order to calm down the tendon before physical therapy is initiated. Anti-inflammatories may be prescribed. Avoiding activities that aggravate the Achilles tendon will help the healing process. Improvement and resolution of symptoms can take months. Exercise might be the cause of Achilles tendonitis, but it can also help prevent it and aid in recovery. Healing will occur more quickly if there is no pressure on the injured tendon, and if the foot is at least partially immobilized.

Surgical Treatment
Surgery for an Achilles tendon rupture can be done with a single large incision, which is called open surgery. Or it can be done with several small incisions. This is called percutaneous surgery. The differences in age and activity levels of people who get surgery can make it hard to know if Achilles tendon surgery is effective. The success of your surgery can depend on, your surgeon's experience. The type of surgery you have. How damaged the tendon is. How soon after rupture the surgery is done. How soon you start your rehab program after surgery. How well you follow your rehab program. Talk to your surgeon about his or her surgical experience. Ask about his or her success rate with the technique that would best treat your condition.
Prevention
While it may not be possible to prevent Achilles tendinitis, you can take measures to reduce your risk. Increase your activity level gradually. If you're just beginning an exercise regimen, start slowly and gradually increase the duration and intensity of the training. Take it easy. Avoid activities that place excessive stress on your tendons, such as hill running. If you participate in a strenuous activity, warm up first by exercising at a slower pace. If you notice pain during a particular exercise, stop and rest. Choose your shoes carefully. The shoes you wear while exercising should provide adequate cushioning for your heel and should have a firm arch support to help reduce the tension in the Achilles tendon. Replace your worn-out shoes. If your shoes are in good condition but don't support your feet, try arch supports in both shoes. Stretch daily. Take the time to stretch your calf muscles and Achilles tendon in the morning, before exercise and after exercise to maintain flexibility. This is especially important to avoid a recurrence of Achilles tendinitis. Strengthen your calf muscles. Strong calf muscles enable the calf and Achilles tendon to better handle the stresses they encounter with activity and exercise. Cross-train. Alternate high-impact activities, such as running and jumping, with low-impact activities, such as cycling and swimming.
 Achilles tendonitis is commonly seen in athletes who sustain an increase in training load, and is most often due to overuse. Tendons respond poorly to overuse, therefore healing is slow. This can leave a tendon pathologically defective, which decreases tendon strength and leaves it less able to tolerate load, thus vulnerable to further injury or tendinosis. Extrinsic factors contributing to this condition include training errors and inappropriate footwear. Intrinsic factors include inflexibility, weakness and malalignment. In other situations, there will be clinical inflammation, but objective pathologic evidence for cellular inflammation is lacking, and in these conditions the term tendinosis is more appropriate. Tendinosis is a degeneration of the tendon?s collagen in response to chronic overuse; when overuse is continued without giving the tendon time to heal and rest, such as with repetitive strain injury, tendinosis results. Even tiny movements, such as clicking a mouse, can cause tendinosis, when done repeatedly.
Achilles tendonitis is commonly seen in athletes who sustain an increase in training load, and is most often due to overuse. Tendons respond poorly to overuse, therefore healing is slow. This can leave a tendon pathologically defective, which decreases tendon strength and leaves it less able to tolerate load, thus vulnerable to further injury or tendinosis. Extrinsic factors contributing to this condition include training errors and inappropriate footwear. Intrinsic factors include inflexibility, weakness and malalignment. In other situations, there will be clinical inflammation, but objective pathologic evidence for cellular inflammation is lacking, and in these conditions the term tendinosis is more appropriate. Tendinosis is a degeneration of the tendon?s collagen in response to chronic overuse; when overuse is continued without giving the tendon time to heal and rest, such as with repetitive strain injury, tendinosis results. Even tiny movements, such as clicking a mouse, can cause tendinosis, when done repeatedly.
Causes
Like any muscle or tendon in the body, the older we get, the more likely we are to sustain an injury. So middle-aged men and women are most at risk, with a slightly higher risk factor attributed to males. Those who participate in more intense athletic activities like high impact sports (tennis, running, basketball) are most susceptible to the injury. Certain underlying medical conditions can also be a contributing factor. Diabetics are more at risk of suffering from Achilles Tendinitis, as are those who are not in great physical shape. Some antibiotics, particularly fluoroquinolones can make one more likely to suffer a strained Achilles Tendon.
Symptoms
Symptoms vary because you can injure various areas of the muscle-tendon complex. The pain may be an acute or chronic sharp, stabbing, piercing, shooting, burning or aching. It is often most noticeable immediately after getting out of bed in the morning, or after periods of inactivity, like sitting down for lunch. After a couple minutes of walking around, it will often then settle down somewhat, before becoming symptomatic again after excessive time standing or walking. But regardless of how the pain is perceived, Achilles tendon pain should not be left untreated due to the danger that the tendon can become weak, frayed, thickened, and eventually it may rupture.
Diagnosis
On examination, an inflamed or partially torn Achilles tendon is tender when squeezed between the fingers. Complete tears are differentiated by sudden, severe pain and inability to walk on the extremity. A palpable defect along the course of the tendon. A positive Thompson test (while the patient lies prone on the examination table, the examiner squeezes the calf muscle; this maneuver by the examiner does not cause the normally expected plantar flexion of the foot).
Nonsurgical Treatment
Treatment depends on severity of pain. The most effective long-term treatment for Achilles tendinitis/tendinopathy is physical therapy, particularly therapy that focuses on eccentric muscle/tendon strengthening. Calf and Achilles stretching are also an important part of the treatment. In severe cases, treatment may begin with a period of rest and immobilization in order to calm down the tendon before physical therapy is initiated. Anti-inflammatories may be prescribed. Avoiding activities that aggravate the Achilles tendon will help the healing process. Improvement and resolution of symptoms can take months. Exercise might be the cause of Achilles tendonitis, but it can also help prevent it and aid in recovery. Healing will occur more quickly if there is no pressure on the injured tendon, and if the foot is at least partially immobilized.

Surgical Treatment
Surgery for an Achilles tendon rupture can be done with a single large incision, which is called open surgery. Or it can be done with several small incisions. This is called percutaneous surgery. The differences in age and activity levels of people who get surgery can make it hard to know if Achilles tendon surgery is effective. The success of your surgery can depend on, your surgeon's experience. The type of surgery you have. How damaged the tendon is. How soon after rupture the surgery is done. How soon you start your rehab program after surgery. How well you follow your rehab program. Talk to your surgeon about his or her surgical experience. Ask about his or her success rate with the technique that would best treat your condition.
Prevention
While it may not be possible to prevent Achilles tendinitis, you can take measures to reduce your risk. Increase your activity level gradually. If you're just beginning an exercise regimen, start slowly and gradually increase the duration and intensity of the training. Take it easy. Avoid activities that place excessive stress on your tendons, such as hill running. If you participate in a strenuous activity, warm up first by exercising at a slower pace. If you notice pain during a particular exercise, stop and rest. Choose your shoes carefully. The shoes you wear while exercising should provide adequate cushioning for your heel and should have a firm arch support to help reduce the tension in the Achilles tendon. Replace your worn-out shoes. If your shoes are in good condition but don't support your feet, try arch supports in both shoes. Stretch daily. Take the time to stretch your calf muscles and Achilles tendon in the morning, before exercise and after exercise to maintain flexibility. This is especially important to avoid a recurrence of Achilles tendinitis. Strengthen your calf muscles. Strong calf muscles enable the calf and Achilles tendon to better handle the stresses they encounter with activity and exercise. Cross-train. Alternate high-impact activities, such as running and jumping, with low-impact activities, such as cycling and swimming.
Painful Feet & Arch Supports
Although itching and blistery feet may be a sign of Athlete's foot, those who have constant numbness or tingling in their feet may be suffering from a condition known as peripheral neuropathy. You can barely remember the last time you weren't bothered by foot pain. For most of us foot pain occurs at sometime in our life. Foot complaining of pain, too often? Foot pain around the ankle is quite common.
There are many conservative treatments for plantar fasciitis that when used accordingly are very successful. Your podiatric physician may refer you to a physical therapist to aid in your treatment and to teach you the most effective stretching techniques for your foot type and condition. You may also be advised to wear a night splint that stretches your tendons and fascia in your foot while you sleep. These treatments can significantly reduce the inflammation of your plantar fascia and thus reduce your pain. You should be wearing shoes that properly stabilize your foot and support your arch. Your podiatric physician can provide you with a prefabricated or custom orthotic that would give your achy foot the support it need. It takes time and therapy to improve the integrity of the tissue.
My web site has been designed to offer information about podiatric Foot care We want you to feel comfortable in ouroffice. Dr. Metzl breaks down what "Plantar Fasciitis" is, how to prevent it, and how to cure it. For 5 to 6 minutes perform as many sets of 15 Rows from Plank, 15 Push-ups, and 15 Sit-ups as possible. Dr. Metzl breaks down what "Runner's Knee" is, how to prevent it, and how to cure it. Dr. Metzl breaks down what IT Band Syndrome is, how to prevent it, and how to cure it. Feet and ankles are built tough, capable of sustaining two or three times our body weight. If your foot is too stiff to bear the impact, a tibial stress fracture could result.
Blood glucose levels under control: Meal planning, regular blood glucose monitoring, substantial activity and right diabetes medications including insulin can all go a long way toward relieving the pain associated with the nerve damage. Look them over: Provide your feet a careful going-over every night to make sure that you haven't developed a cut, scrape, sore, blister or any other tiny problem.
I recently stopped wearing them for a few months, and the heel pain returned, so I'm ordering more for my shoes. When I initially put your inserts into my shoes, they felt a bit strange, especially in my arches. Shoes with high heels can create much trouble for your feet.
Participants were asked to indicate when the sensation of pressure changed to onset of pain. The paper grip test was used as a clinical measure of hallux plantarflexion strength 38 , 39 Participants completed three trials of three seconds, and a pass was recorded if the individual could hold the paper under the hallux against resistance for all trials.
There are also many muscles, tendons and ligaments within your foot. The bones, ligaments and tendons within your foot form the foot arches. These arches are called the longitudinal and transverse arches. It is your foot arches that allow your foot to hold up the weight of your body. Nerves also provide sensation to the skin of your foot. Metatarsalgia is a general name given to pain in the front part of your foot under the heads of your metatarsal bones. The pain can occur in one or both feet.
There are many conservative treatments for plantar fasciitis that when used accordingly are very successful. Your podiatric physician may refer you to a physical therapist to aid in your treatment and to teach you the most effective stretching techniques for your foot type and condition. You may also be advised to wear a night splint that stretches your tendons and fascia in your foot while you sleep. These treatments can significantly reduce the inflammation of your plantar fascia and thus reduce your pain. You should be wearing shoes that properly stabilize your foot and support your arch. Your podiatric physician can provide you with a prefabricated or custom orthotic that would give your achy foot the support it need. It takes time and therapy to improve the integrity of the tissue.
My web site has been designed to offer information about podiatric Foot care We want you to feel comfortable in ouroffice. Dr. Metzl breaks down what "Plantar Fasciitis" is, how to prevent it, and how to cure it. For 5 to 6 minutes perform as many sets of 15 Rows from Plank, 15 Push-ups, and 15 Sit-ups as possible. Dr. Metzl breaks down what "Runner's Knee" is, how to prevent it, and how to cure it. Dr. Metzl breaks down what IT Band Syndrome is, how to prevent it, and how to cure it. Feet and ankles are built tough, capable of sustaining two or three times our body weight. If your foot is too stiff to bear the impact, a tibial stress fracture could result.
Blood glucose levels under control: Meal planning, regular blood glucose monitoring, substantial activity and right diabetes medications including insulin can all go a long way toward relieving the pain associated with the nerve damage. Look them over: Provide your feet a careful going-over every night to make sure that you haven't developed a cut, scrape, sore, blister or any other tiny problem.
I recently stopped wearing them for a few months, and the heel pain returned, so I'm ordering more for my shoes. When I initially put your inserts into my shoes, they felt a bit strange, especially in my arches. Shoes with high heels can create much trouble for your feet.

Participants were asked to indicate when the sensation of pressure changed to onset of pain. The paper grip test was used as a clinical measure of hallux plantarflexion strength 38 , 39 Participants completed three trials of three seconds, and a pass was recorded if the individual could hold the paper under the hallux against resistance for all trials.

There are also many muscles, tendons and ligaments within your foot. The bones, ligaments and tendons within your foot form the foot arches. These arches are called the longitudinal and transverse arches. It is your foot arches that allow your foot to hold up the weight of your body. Nerves also provide sensation to the skin of your foot. Metatarsalgia is a general name given to pain in the front part of your foot under the heads of your metatarsal bones. The pain can occur in one or both feet.
